Abstract
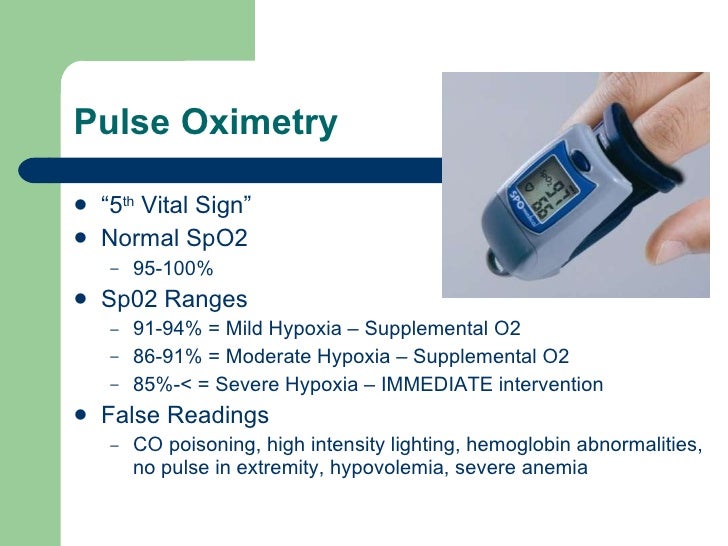
SpO2 is another oxygen level. It’s the percentage of oxygen molecules you inhale that make it to your arterial blood. A perfectly normal value is 98%. However, anything greater than 90% is considered acceptable. – A patient with a true saturation of 90% could have a SpO2 value displayed of 94% (+/-3%) or 86% (+/-3%). – With a SpO2 display of 90% the patient could have a.
Across the world healthcare systems are dealing with COVID 19. One of the main manifestations of this infection is varied degree of involvement of lung causing a spectrum of illness from mild lower respiratory tract infection to severe Adult Respiratory Distress Syndrome (ARDS). One of the important clinical parameters is to identify hypoxia early to initiate higher level of care at the earliest. However, presence of silent or latent hypoxia has made this task a challenge in COVID 19. A simple 6-minute walk test (6MWT) to look for inducible hypoxia for a patient who looks comfortable and is not hypoxic at rest, helps in early detection of hypoxia and initiating early higher-level care. The 6MWT also helps in looking for discharge preparedness of patient. This simple tool has immense clinical applicability to ensure safe care of COVID 19 patients.
COVID 19 has manifested in several forms but to unmask latent hypoxia is the key to save lives and its imperative to have an easy clinical tool to screen for the same. While many protocols have been developed for risk stratification like National Early Warning Signs 2 (NEWS 2), SOFA score neither have the ability to predict hypoxia. Pulmonary manifestation of covid19 can be easily picked up by a simple user friendly 6 miniute walk test which can detect desaturation to pick up silent hypoxia which has been often referred to as “happy hypoxia”.1 Another observation in COVID 19 patients is at rest they appear comfortable and saturation are maintained above 94%, however mild exertion like using washroom often makes them hypoxic and/or short of breath. Thus, in this group of patients, it is important to identify hypoxia early, stratify the risk and plan treatment.
A simple 6 minutes’ walk test (6MWT)2 is a reliable tool to assess cardiorespiratory effort tolerance in chronic lung and chronic heart failure patients. Traditionally the test involves measuring the heart rate and blood pressure along with oxygen saturation using a finger pulse oximeter probe. Jenkins et al3 proposed a stopping criterion for the test based on drop in the measured oxygen saturation (SpO2) by finger probe. The test provides a global assessment of the cardio-pulmonary reserves. A simple effort of walking at a steady pace in patients with compromised cardio respiratory reserves may precipitate a drop in oxygen saturation. There are many physiological variables which may be attributed to drop in saturation, however the most important been hearts inability to improve cardiac output and second, decrease in lung diffusion capacity which can be due to lung infiltration due to COVID 19 pneumonia and/or due to alveolar capillary micro thrombi in the pulmonary circulation (pulmonary vascular endothilitis).4 The 6-minute walk test can also predict the anaerobic threshold in patients. Anaerobic threshold is a reflection of combine efficiency of heart, lung and circulation and marks the onset of anaerobic metabolism due to oxygen deficit secondary to inadequate oxygen delivery. Sinclair et al5 in 110 patients used 6MWT to derive the anaerobic threshold in patients awaiting non cardiac surgery.
A classic 6-minute walk test (6MWT)as described in American Thoracic Society statement6 is used for measuring response to medical interventions in patients with moderate to severe cardiac or pulmonary disease, it assesses one-time functional status of patient and predict morbidity and mortality. The principle of 6-minute walk test in COVID 19 is to identify patients who are not hypoxic at rest, but become hypoxic (silent Hypoxia) on 6-minute walk test. The 6MWT will ascertain evidence of hypoxia identified by SpO2 less than 94% or an absolute drop in SpO2 by more than 3% from base line during or at end of the test. Patients over 60 years of age may have a shorter- 3-minute walk test (3MWT) if they are unable to perform a 6-minute test. The test is indicated in all COVID-19 positive patients who are not hypoxic or short of breath at rest. The test is contraindicated if patient is hypoxic at rest SpO2 < 94 %, Short of breath at rest, not able to walk unassisted, Eisenmenger’s syndrome, severe anaemia, known patient of unstable angina or valvular heart disease.
The 6MWT can be performed at home or hospital, one person either family member or healthcare worker supervises the test. Patient fulfils the prerequisite indication to identify latent or silent hypoxia and there is no contraindication. Patient is requested to wear a simple cloth or three-ply mask. A base line saturation using finger pulse oximeter probe is noted. Patient is requested to start walking in confines of his room, it is a self-paced test, and patient can do as many laps as he can in confines of room. At end of 6 minutes a repeat reading of saturation is taken, a positive test for hypoxia is if SpO2 is less than 94% or there is an absolute drop of SpO2 by 3% or more from baseline. If patient feels lightheaded, unwell or short of breath during the walk, then test should be aborted, patient rested and SpO2 checked. Similarly, patients over 60 years of age, an interim reading of SpO2 at 3 minutes and supervisor of test assessing the need to complete 6 minutes or stop is mandatory.
A positive test mandates higher level care, this means patients who are home quarantined need to present to emergency department of hospital, similarly on treatment ward patients may need to be shifted to High Dependency Unit (HDU) or Intensive Care Unit (ICU). The test also helps doctors to seek additional laboratory information like CRP, D-dimer, Ferritin and IL6 as needed. The test should be repeated again closer to discharge day to assess discharge readiness, it assesses cardiorespiratory reserve post recovery and completes a comprehensive clinical assessment for readiness to discharge. Giannitis et al7 proposed to do the test closer to discharge day in patients with heart failure to assess the cardio respiratory functional status of the patient.
Summary
The 6MWT is a simple and effective test to assess the silent hypoxia, it helps in identifying patients early who have a potential to deteriorate. This simple intervention would help in initiating appropriate esclation of level of care and treatment. The ease of doing a self paced test may be tempting, but it needs to be performed under supervision and if positive for hypoxia then necessary action needs to be initiated. It can also be used to assess discharge readiness. The simplicity, improvement of margin of safety and prompting early intervention make this test an important tool in COVID 19 patient management.
References
- Wilkerson RG, Adler JD, Shah NG, et al. Silent hypoxia: A harbinger of clinical deterioration in patients with COVID-19. Am J Emerg Med 2020 May 22.
- Singh SJ, Puhan MA, Andrianopoulos V, et al. An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease. Eur Respir J 2014; 44:1447–1478.
- Jenkins S, Cecins N . Six-minute walk test: observed adverse events and oxygen desaturation in a large cohort of patients with chronic lung disease. Intern Med J 2011; 41:416–22.
- Ackermann M, Verleden SE et al Pulmonary vascular endothilitis, thrombosis and angiogenesis in COVID -19. N Engl J Med 2020; 383:120-128.
- Sinclair RC, Batterham AM, Davies S, Cawthorn L, Danjoux GR. Validity of the 6 min walk test in prediction of the anaerobic threshold before major non-cardiac surgery. Br J Anaesth 2012; 108:30–35.
- American Thoracic Society (ATS) Statement: Guidelines for Six-minute walk test. Am J Respir Crit Care Med 2002; 166:111–117.
- Giannitsi S, Bougiaklo M, Bechlioulis A, Kotsia A, Michalis LK, Naka KK. 6 minute walk test:a useful tool in the management of heart failure patients. Ther Adv Cardiovasc Dis 2019; 13.
Blood oxygen levels during sleep should be at a 95 percent saturation, which is considered normal, according to the American Sleep Apnea Association (AASM).
It is normal for blood oxygen levels to decrease during sleep. All body systems have altered basal function during your sleep, including breathing. You don’t breathe as deeply when you are sleeping, and not all your lung spaces function at full capacity. Because of this effect of sleep on breathing, it is normal for your sleep oxygen level to decrease below awake levels. Tests that show a waking oxygen level at or above 94 percent typically indicate a sleep oxygen level of at or above 88 percent.
However, when it persistently drops below maintenance levels, health problems can develop. In addition, certain medical conditions can lead to low oxygen while you are asleep.
Medical Disorders
According to the Mayo Clinic, certain medical problems, especially of the cardiovascular and respiratory systems, can lead to blood oxygen below normal levels. The effects of these conditions can worsen while you are sleeping. The most common disorders include:
Diseases of the lungs:
Several lung diseases can narrow or block lung air spaces, inflame or scar lung tissue, and can also interfere with normal breathing patterns. These lung diseases include:
- Chronic obstructive pulmonary disease (COPD), such as emphysema and chronic bronchitis
- Asthma
- Cystic fibrosis, a genetic disease that causes a build of mucus in the lungs
- Pneumonia and other lung infections
- Smoking and lung cancer
Heart diseases:
Disorders of the heart, which can interfere with blood flow, blood oxygen level, and oxygen supply to tissues include:
- Coronary heart disease, a build-up of plaques in the arteries of the heart
- Congestive heart failure with leakage of fluid into lung tissue
- Congenital heart disease, a developmental defect in the structure of the heart
Anemia:
The decrease in hemoglobin (Hgb) with anemia lowers the ability of your red blood cells to absorb oxygen from your lungs and carry it to your tissues. Abnormal Hgb, such as with sickle cell anemia, causes the same problem.
Obesity:
This a cause of sleep apnea where the throat becomes obstructed during sleep and interferes with breathing. Obesity also causes obesity hypoventilation syndrome (OHS), with diminished deep breathing and oxygen intake.
Drugs:
Chronic use of prescription or illegal opioids, sedatives, and recreational or other illegal drugs can depress the brain’s breathing center and therefore slow down your breathing and oxygen intake.
Alcohol:
Abuse of alcohol, especially at bedtime and mixed with drugs, can interfere with normal breathing and sufficient oxygen intake.
94 Spo2 While Sleeping
Health Consequences
A normal blood oxygen level is vital for normal tissue and cellular function. Therefore, low blood oxygen affects the function of every tissue in the body. A chronic problem of low oxygen levels while sleeping can increase the risk for several health consequences including:
- Sleep disorders, such as bouts of insomnia
- Poor sleep quality, such as restless sleep with several awakenings
- High blood pressure
- Cardiovascular disease including heart failure
- Cardiac arrhythmia and a risk for sudden death
- Type 2 diabetes
- Depressed brain function and possible brain damage
- Risk for loss of consciousness, coma, and death
94 Spo2 87 Pr Bpm
If you think your oxygen level falls below normal while you are sleeping, consult with your doctor. He might suggest a sleep study as part of your evaluation. During an overnight stay in a sleep center, a technician monitors your breathing and other signs, as well as your blood O2 sat with a pulse oximeter during sleep.
